- Home
-
Services
- Autism Assessments >
- Coaching
- Couples >
- Discernment Counseling
- Educational Consulting | Special Needs Advocacy >
- Psychiatric Services | Medication Management
- Nutrition
- Parenting + Family Therapy
- Play Therapy for Children
- Separation Counseling + Collaborative Parenting
- Telehealth
- Therapy for Teachers
- Trauma
- Schedule Appointment
-
Meet the Team
- Abby Olmstead
- Adrienne Fisher
- Amber Garcia >
- Amber Miner
- Andrea Miles
- Arionna Wilkerson
- Autumn Martin
- Amber Miner
- Brittany Kai
- Brittany Proxmire
- Brittany Stewart
- Bru Ramirez >
- Chantal D. Hayes
- Christine Ridley
- Emily Ortiz Badalamente
- Hayley McCraw
- Jamie Cullen
- Jared Brinkerhoff
- Jordan Peterson
- Josh Bolle
- Les Gura
- Lisa Carpenter
- Logan King
- Rashaad Nelson
- Sarah Vanderpool
- Savannah Ornt
- Simone Banks
- Tiffany Woods
- Administrative Staff >
- About Us
- Hiring
|
In the practice of psychotherapy, therapists learn about and utilize many tools to help our clients find lasting change, improving their overall mental health and wellbeing, and psychotropic medications can be one of those tools. It is important to realize that not everyone needs medication to treat their mental health symptoms, and not everyone who needs medication will need it forever. The purpose of this article is to provide basic education about psychotropic medications, because I find that most of my clients who take psychotropic medications are under-educated about them, and many clients who do not take medications are scared to start for the same reason. How do psychotropic medications affect the brain?Mental health disorders (anxiety, depression, bipolar disorder, etc…) are a result of chemical imbalances in the brain, specifically of the neurotransmitters serotonin, norepinephrine and dopamine. These chemical imbalances can be endogenous (genetic factors, internally caused), exogenous (life events, trauma, external factors), or both. Psychotropic medications work to create balance in neurotransmitters by adjusting how the receptors in the brain absorb the chemical, effectively reducing negative symptoms. Different medications work on different neurotransmitters, and it varies individually what each person’s brain needs or will respond to, depending on symptoms and brain chemistry. What are the types of psychotropic medication? Anti-Anxiety Medications
Anti-Depressant Medications
Antipsychotic Medications Used to treat Bipolar Disorder, Schizophrenia, Personality Disorders, Severe Depression and Severe Anxiety.
Mood Stabilizers Used to treat the mood swings of Bipolar Disorder, and sometimes to enhance the effect of other medications when treating Depression. Reduce excitability in the brain, to calm overstimulated and overactive neurons. Many anticonvulsant medications are used as mood stabilizers. Examples: Lithium (Eskalith), Depakote (Divalproex Sodium), Lamictal (Lamotrigine), Tegretol (Carbamazepine), Topamax (Topiramate), Trileptal (Oxcarbazepine) Stimulants Used to treat Attention Deficit Hyperactivity Disorder (ADHD), increase dopamine and norepinephrine. Can be addictive and can easily form a dependence. Examples: Adderall (Amphetamine), Vyvanse (lisdexamfetamine), Focalin (dexmethylphenidate), Ritalin/Concerta (methylphenidate), Dexedrine (dextroamphetamine) Who can prescribe psychotropic medications? While a licensed therapist or counselor may be knowledgeable about psychotropic medications, only medical professionals can prescribe them. The medical professionals with the most knowledge and training in prescribing psychoactive medications are Psychiatrists. Psychiatrists are medical doctors (MD) that have completed residency and training in psychiatry. Most psychiatrists do not engage in talk therapy; they focus on symptom and medication management in brief (15-20 minute) appointments. Other medical professionals able to prescribe psychotropic medications are Primary Care Physicians (MD/GP), Physician Assistants (PA), Psychiatric/Mental Health Nurse Practitioners (PMHNP), Nurse Practitioners (NP), Certified Nurse Midwives (CNM), and Gynecologists/Obstetricians (OB/GYN). How do I know if I need psychotropic medications? In my practice, for someone who is not currently taking psychotropic medications, I will generally recommend medications if we seem to continue hitting a wall with ongoing negative symptoms, despite all reasonable efforts to improve them. If adding structure, recognizing and changing thinking, improving overall physical health, learning emotional identification and expression, and addressing spiritual health doesn’t improve symptoms markedly, this indicates to me that the symptoms are endogenous in nature, and need chemical help to mitigate. What do I need to be aware of if I start taking psychotropic medications? All medications generally have some risk of side-effects, some more troublesome than others. Speaking with your prescribing physician and doing your own research are important before starting on any psychotropic medication. Most common side-effects for psychotropic medications are disturbances in sleep and appetite. Some of these can be mitigated by adjusting the time of day they are taken (morning if the medication is activating to your brain at night), and taking them with food to reduce nausea. Research has shown that the most effective treatment for mental health disorders is a combination of medication and therapy. Taking psychotropic medications without including therapy will not result in lasting change and improvement in symptoms. For real and sustained life change, medications can help provide enough of a lift or relief of symptoms so work can happen in therapy, to prevent recurrence of negative symptoms.
2 Comments
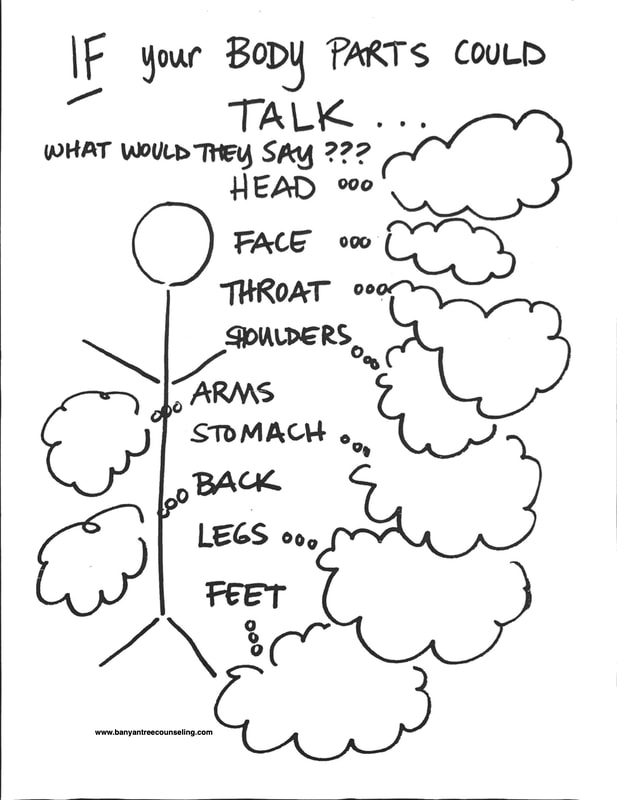
If your body parts could talk, what would they say?I've used this worksheet with my own children, with students I've taught, and with clients, both children and adults. Teaching kids to "tune in" to their bodies is an essential skill and doesn't always come naturally. There are so many benefits to learning this skill! One is emotional regulation-- kids who can listen to their body have an easier time managing and coping with their feelings, especially the really big ones, like anger, disappointment, fear, frustration, guilt, sadness.. . They feel more capable, confident, have a more secure sense of self. They have less behavioral problems, better social skills with peers, more empathy and supportive relationships... It's not just a skill for kids., Adults benefit in similar ways, too, with overall mental stability, positive sense of self, solid relationships, increased career satisfaction. Take a moment today to tune inward,. Breathe in for 4 seconds, hold for 7, and slowly release for 8. Then scan your body and really listen to what each body part is telling you. Maybe some are silent, while others are screaming! That's ok, no judgement. All you have to do is listen. Click to download the PDF to use at home.
Are you worried about your anxious child? |
Banyan Tree Counseling & WellnessWe are a team of licensed clinicians with a holistic, strengths-based, and evidence-based approach. We offer counseling for people of all ages, life coaching, group therapy, educational consulting and advocacy, assessments, and dietary nutrition services. Categories
All
|
||||||||
Individual Counseling • Psychiatric Services • Medication Management • Nutrition counseling
COUPLES & FAMILIES • CHILDREN & TEENS • EDUCATIONAL ADVOCACY
If you are in a life threatening situation call 1 (800) 273-8255 or use these resources to get immediate help.
HIPAA Notice of Privacy Practices
© 2015-2024 Banyan Tree Counseling PLLC | Banyan Integrated Health PLLC | Banyan Tree Wellness LLC | All Rights Reserved.
All content on this website, unless otherwise specified, is the sole property of Banyan Tree Counseling & Wellness and is protected by copyright laws.
Any unauthorized reproduction, distribution, or use of this content is strictly prohibited and may result in legal action.
HIPAA Notice of Privacy Practices
© 2015-2024 Banyan Tree Counseling PLLC | Banyan Integrated Health PLLC | Banyan Tree Wellness LLC | All Rights Reserved.
All content on this website, unless otherwise specified, is the sole property of Banyan Tree Counseling & Wellness and is protected by copyright laws.
Any unauthorized reproduction, distribution, or use of this content is strictly prohibited and may result in legal action.
- Home
-
Services
- Autism Assessments >
- Coaching
- Couples >
- Discernment Counseling
- Educational Consulting | Special Needs Advocacy >
- Psychiatric Services | Medication Management
- Nutrition
- Parenting + Family Therapy
- Play Therapy for Children
- Separation Counseling + Collaborative Parenting
- Telehealth
- Therapy for Teachers
- Trauma
- Schedule Appointment
-
Meet the Team
- Abby Olmstead
- Adrienne Fisher
- Amber Garcia >
- Amber Miner
- Andrea Miles
- Arionna Wilkerson
- Autumn Martin
- Amber Miner
- Brittany Kai
- Brittany Proxmire
- Brittany Stewart
- Bru Ramirez >
- Chantal D. Hayes
- Christine Ridley
- Emily Ortiz Badalamente
- Hayley McCraw
- Jamie Cullen
- Jared Brinkerhoff
- Jordan Peterson
- Josh Bolle
- Les Gura
- Lisa Carpenter
- Logan King
- Rashaad Nelson
- Sarah Vanderpool
- Savannah Ornt
- Simone Banks
- Tiffany Woods
- Administrative Staff >
- About Us
- Hiring